Argoty Pantoja A.D., Velázquez Cruz R., Meneses León J., Salmerón J., Rivera Paredez B. (2023) Triglyceride-glucose index and incident hypertension in Mexican adults: Up to 13 years’ follow-up. Lipids in Health and Disease 22, 162. |
 Azur M.J., Stuart E.A., Frangakis C., Leaf P.J. (2011) Multiple imputation by chained equations: What is it and how does it work?. International Journal of Methods in Psychiatric Research 20, 40-49. |
 Ballena-Caicedo J., Zuzunaga-Montoya F.E., Loayza-Castro J.A., Vásquez-Romero L. E. M., Tapia-Limonchi R., Gutierrez De Carrillo C. I., Vera-Ponce V. J. (2025) Global prevalence of dyslipidemias in the general adult population: A systematic review and meta-analysis. Journal of Human Nutrition and Public Health 10, 118-125. |
 Brennan A.T., Getz K.D., Brooks D.R., Fox M.P. (2021) An underappreciated misclassification mechanism: Implications of nondifferential dependent misclassification of covariate and exposure. Annals of Epidemiology 58, 104-123. |
 Cox D.R. (1972) Regression models and life-tables. Journal of the Royal Statistical Society: Series B 34, 187-220. |
 Desquilbet L., Mariotti F. (2010) Dose-response analyses using restricted cubic spline functions in public health research. Statistics in Medicine 29, 1037-1057. |
 Gao Y., Yu L., Li X., Yang C., Wang A., Huang H. (2021) The effect of different traditional Chinese exercises on blood lipid in middle-aged and elderly individuals: A systematic review and network meta-analysis. Life (Basel) 11, 714. |
 Gounden V., Devaraj S., Jialal I. (2024) The role of the triglyceride-glucose index as a biomarker of cardio-metabolic syndromes. Lipids in Health and Disease 23, 416. |
 Hansson G. K. (2005) Inflammation, atherosclerosis, and coronary artery disease. New England Journal of Medicine 352, 1685-1695. |
 Hartley L., Flowers N., Lee M.S., Ernst E., Rees K. (2014) Tai chi for primary prevention of cardiovascular disease. Cochrane Database Syst Rev 2014, CD010366. |
 Ho S.S., Dhaliwal S.S., Hills A.P., Pal S. (2012) The effect of 12 weeks of aerobic, resistance or combination training on cardiovascular risk profile. BMC Public Health 12, 704. |
 Huang Y., Gao L., Xie X., Tan S.C. (2014) Epidemiology of dyslipidemia in Chinese adults: Pooled estimates. Popul Health Metr 12, 23. |
 Kaplan E.L., Meier P. (1958) Nonparametric estimation from incomplete observations. Journal of the American Statistical Association 53, 457-481. |
 Khan S.H., Sobia F., Niazi N.K. (2018) Triglyceride-glucose index: A reliable marker for insulin resistance. Diabetology and Metabolic Syndrome 10, 74. |
 Kirkwood, B.R. and Sterne, J.A.C. (2003) Essential Medical Statistics.
2nd ed. Blackwell. |
 Knol M.J., VanderWeele T.J. (2012) Presenting analyses of effect modification and interaction. International Journal of Epidemiology 41, 514-520. |
 Krüger K., Mooren F.C., Pilat C. (2022) The immunological effects of exercise in preventing dyslipidemia and cardiovascular disease. Frontiers in Physiology 13, 903713. |
 Li J.J., Zhao S.P., Zhao D., Liu L.S., Lu G.P., Gu D.F., Yu B L., Wang W., Liu J., Li Y.H., Hu D.Y., Dong Q., Xie W., Cui C.J., Yang Y. J., Zhu J.R., Jiang L.X., Lu H.S., Liu M.M. (2023) 2023 Chinese guideline for lipid management. Frontiers in Pharmacology 14, 1190934. |
 Li Y., Zhai Q., Li G., Peng W. (2024) Effects of different aerobic exercises on blood lipid levels in middle-aged and elderly people: A systematic review and Bayesian network meta-analysis based on randomized controlled trials. Healthcare 12, 1309. |
 Little, R.J.A. and Rubin, D.B. (2019) Statistical Analysis with Missing
Data. 3rd ed. Wiley. |
 Lu Y., Wang H., Feng Z., Mu J., Schulz H., Ding J., Yang X., Li X., Hu D. (2021) Prevalence of dyslipidemia and availability of lipid-lowering medications among primary health care settings in China. JAMA Netw Open 4, e2127573. |
 Mathur M.B., VanderWeele T.J. (2020) Sensitivity analysis for unmeasured confounding in meta-analyses. Journal of the American Statistical Association 115, 163-172. |
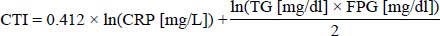
 Mei Y., Li Y., Zhang B., Xu R., Feng X. (2024) Association between the C-reactive protein-triglyceride glucose index and erectile dysfunction in US males: Results from NHANES 2001-2004. International Journal of Impotence Research 37, 612-622. |
 Meng X., D’Arcy C. (2020) Physical activity trajectories and health outcomes among middle-aged and older Chinese adults: Evidence from CHARLS. BMJ Open 10, e034603. |
 O’Brien R.M. (2007) A caution regarding rules of thumb for variance inflation factors. Quality and Quantity 41, 673-690. |
 Opoku S., Gan Y., Addo Yobo E., Tenkorang-Twum D., Yue W., Wang Z., Lu Z. (2021) Awareness, treatment, control, and determinants of dyslipidemia among adults in China: Results from the China National Stroke Screening and Prevention Project (CNSSPP). Scientific Reports 11, 10056. |
 Orsini N., Greenland S. (2011) Tabulation and plotting after flexible modeling of a quantitative covariate. Stata Journal 11, 1-29. |
 Pandey A., Salahuddin U., Garg S., Ayers C., Kulinski J., Anand V., Mayo H., Kumbhani D.J. (2016) Continuous dose-response association between sedentary time and risk for cardiovascular disease: A meta-analysis. JAMA Cardiology 1, 575-583. |
 R Core Team. (2022) R: A Language and Environment for Statistical
Computing. R Foundation, Vienna. |
 Ridker P.M. (2003) High-sensitivity C-reactive protein: A novel and important marker of cardiovascular risk. Circulation 107, 363-369. |
 Ridker P.M. (2007) C-reactive protein and the prediction of cardiovascular events. American Journal of Medicine 120, 21-24. |
 Roth G. A., Men sah G. A., Johnson C. O. (2020) Global burden of cardiovascular diseases and risk factors, 1990-2019: Update from the GBD 2019 Study. Journal of the American College of Cardiology 76, 2982-3021. |
 Rothman, K.J., Greenland, S. and Lash, T.L. (2008) Modern
Epidemiology. 3rd ed. Lippincott Williams & Wilkins. |
 Ruan G.T., Xie H.L., Zhang H.Y., Liu C.A., Ge Y.Z., Zhang Q., Wang Z.W., Zhang X., Tang M., Song M.M., Zhang X.W., Yang M., Chen Y.B., Yu K.Y., Deng L., Gong Y.Z., Hu W., Wang K. H., Cong M.H., Shi H.P. (2022) A novel inflammation- and insulin resistance-related indicator to predict the survival of patients with cancer. Frontiers in Endocrinology 13, 905266. |
 Shoelson S.E., Lee J., Goldfine A.B. (2006) Inflammation and insulin resistance. Journal of Clinical Investigation 116, 1793-1801. |
 Simental-Mendía L.E., Rodríguez-Morán M., Guerrero-Romero F. (2008) The product of fasting glucose and triglycerides as surrogate for identifying insulin resistance in apparently healthy subjects. Journal of Clinical Endocrinology and Metabolism 93, 3347-3351. |
 Smart N.A., Downes D., van der Touw T., Hada S., Dieberg G., Pearson M.J., Wolden M., King N., Goodman S.P.J. (2025) The effect of exercise training on blood lipids: A systematic review and meta-analysis. Sports Medicine 55, 67-78. |
 Sterne J.A.C., White I.R., Carlin J.B., Spratt M., Royston P., Kenward M.G., Wood A.M., Carpenter J.R. (2009) Multiple imputation for missing data in epidemiological and clinical research: Potential and pitfalls. BMJ 338, b2393. |
 Tang S., Zhang Y., Liu L., Wang H., Li K., Chen Y., Zheng Q., Meng J., Chen X. (2024) C-reactive protein-triglyceride-glucose index predicts stroke in hypertensive patients. Diabetology & Metabolic Syndrome 16, 1529. |
 Therneau, T.M. and Grambsch, P.M. (2000) Modeling Survival Data:
Extending the Cox Model. Springer. |
 Vandenbroucke J.P., Pearce N. (2012) Case-control studies: Basic concepts. International Journal of Epidemiology 41, 1480-1489. |
 VanderWeele T.J., Ding P. (2017) Sensitivity analysis in observational research: Introducing the E-value. Annals of Internal Medicine 167, 268-274. |
 Wang Y., Xu D. (2017) Effects of aerobic exercise on lipids and lipoproteins in adults: A meta-analysis. Lipids in Health and Disease 16, 132. |
 Wu J., Yang L., Ye J., Ran L., Xu Y.Q., Zhou N. (2022) Sedentary time and cardiovascular disease risk: Systematic review and meta-analysis. BMC Public Health 22, 12728. |
 Xia Q., He X., Liu J., Liu W., Zhang H., Zhang Y., Zhao Y. (2023) Prevalence, awareness, treatment, and control of dyslipidemia in mainland China: A systematic review and meta-analysis. Frontiers in Cardiovascular Medicine 10, 1186330. |
 Xu M., Zhang L., Xu D., Shi W., Zhang W. (2024) Usefulness of C-reactive protein-triglyceride glucose index in detecting prevalent coronary heart disease: Findings from the National Health and Nutrition Examination Survey 1999-2018. Front Cardiovasc Med 11, 1485538. |
 Zhang Z., Guo H., Sun Z., Zhang D., Lin Y., Huang L., Guo Z., Tan L. (2025) Modified TyG indices and TG/HDL-C with all-cause and cause-specific mortality in UK Biobank. Lipids in Health and Disease 24, 126. |
 Zhou Z., Tian X. (2024) Prevalence and association of sleep duration and different volumes of physical activity with type 2 diabetes: First evidence from CHARLS. BMC Public Health 24, 3331. |
 Zhao S., Zhong J., Sun C., Zhang J. (2021) Effects of aerobic exercise on TC, HDL-C, LDL-C and TG in patients with hyperlipidemia: A protocol of systematic review and meta-analysis. Medicine (Baltimore) 100, e25103. |
 Zhao Y., Hu Y., Smith J. P., Strauss J., Yang G. (2014) Cohort profile: The China Health and Retirement Longitudinal Study (CHARLS). International Journal of Epidemiology 43, 61-68. |
 Zhao, Y., Strauss, J., Chen, X., Wang, Y., Gong, J., Meng, Q., Wang, G.,
and Wang, H. (2020) China Health and Retirement Longitudinal
Study—2011-2018 National Baseline and Follow-up Users’
Guide. National School of Development, Peking University.
|
|