|
|
|
| |
| ABSTRACT |
|
Osgood-Schlatter disease (OSD) is caused by high, repetitive, and continuous traction exerted by the quadriceps on the tibial tuberosity, primarily occurring in adolescents. Infrapatellar straps are commonly recommended for its prevention and treatment, yet their impact on quadriceps forces in adolescents remains unstudied. Furthermore, current research on OSD predominantly focuses on adolescent males, with limited attention to adolescent females, despite similar incidence rates in both groups. This study aimed to quantify the quadriceps forces during running, both with and without infrapatellar straps, in adolescent females. Kinematic data, ground reaction forces, and electromyography (EMG) data of knee muscles from 16 adolescent females were recorded as they ran at self-selected speeds with and without infrapatellar straps. OpenSim was employed to estimate quadriceps activations and forces, from which accumulated forces were derived. The simulation's reliability was validated by calculating the correlation between muscle activations obtained from OpenSim and EMG data, which revealed a strong correlation. Wearing infrapatellar straps during running decreased the peak and accumulated forces of the quadriceps (p < 0.001, and p < 0.001, respectively). The significant reduction in accumulated forces was associated with decreased vastus muscle forces during the stance phase (p = 0.002, p = 0.003, and p = 0.016 for vastus lateralis, vastus medialis, and vastus intermedius, respectively). The use of infrapatellar straps had limited effect on the rectus femoris muscle forces. The reliability of the simulation was validated through EMG data. Wearing infrapatellar straps may reduce the load exerted on the tibial tuberosity by decreasing vastus muscle forces during the stance phase. Adolescents aiming to reduce excessive rectus femoris muscle forces due to a shortened or tight rectus femoris, which may contribute to the occurrence of OSD, might experience limited benefits from wearing infrapatellar straps. |
| Key words:
Osgood-Schlatter disease, inverse dynamics simulation, accumulated force
|
Key
Points
- The peak and accumulated forces of the quadriceps decreased when running with infrapatellar straps.
- The reduction in the accumulated forces of the quadriceps was strongly associated with the reduction in vastus muscle forces during the stance phase of the gait cycle.
- Wearing infrapatellar straps during running had little effect on the forces exerted by the rectus femoris.
- The use of infrapatellar straps during running is beneficial for managing Osgood-Schlatter disease, particularly in adolescent females who need to reduce excessive vastus muscle forces.
- Adolescent females aiming to reduce excessive rectus femoris muscle forces may experience limited benefits from wearing infrapatellar straps during running.
|
Osgood-Schlatter disease (OSD) is a traction apophysitis of the knee characterized by localized pain and swelling at the tibial tuberosity (Rathleff et al., 2020). The disease develops between the ages of 10-15 years in boys and 8-14 years in girls (Itoh et al., 2018). Approximately 9.8% of adolescents are affected by OSD, with a higher prevalence among those who participate in high-risk sports that require running, jumping, and kicking (de Lucena et al., 2011; Takei et al., 2023). OSD is commonly described as a self-limiting disease that resolves within 12-18 months or ultimately with growth (Rathleff et al., 2020). However, symptoms related to OSD may persist into adulthood, impacting the daily lives and sports activities of young adults with a history of OSD (Guldhammer et al., 2019). Therefore, effective intervention for OSD and the implementation of preventive measures before its onset are of great importance. OSD is predominantly treated conservatively because it occurs in adolescents who are in the growth phase (Neuhaus et al., 2021). Infrapatellar straps have been recommended for over 40 years as a treatment to alleviate anterior knee pain caused by various conditions, including OSD (Lavagnino et al., 2011). Uzunov, 2008; Mital and Matza, 1977 recommended using infrapatellar straps as a conservative treatment for managing OSD during activities. Adirim et al. (2003) pointed out that knee straps are often beneficial for athletes as they reduce the traction forces on the tibial tubercle. Although the above-mentioned studies recommend the use of infrapatellar straps, their effectiveness on the treatment and prevention of OSD was not investigated in these researches. To the best of the author's knowledge, only one study has investigated the clinical effectiveness of infrapatellar straps in managing OSD. Levine and Kashyap, 1981 studied 17 OSD patients (24 knees) who wore infrapatellar straps during activity. Results showed that 19 affected knees (79.1%) improved after six to eight weeks. The authors speculated that infrapatellar straps work by reducing the pull of the quadriceps applied on the tibial tuberosity. However, quadriceps forces on the tibial tuberosity were not evaluated in their study. It is widely accepted that OSD is caused by the high, repeated, and continued traction of quadriceps (Bezuglov et al., 2020; Ladenhauf et al., 2020; Uzunov, 2008). Although some studies have indicated that infrapatellar straps may reduce the force or the load on the tibial tuberosity (Dar and Mei-Dan, 2019; Lavagnino et al., 2011; Toonstra and Cripps, 2020), the authors have not provided quantitative assessments of the effect of infrapatellar straps on the load. To the authors' knowledge, the impact of infrapatellar straps on quadriceps forces during dynamic tasks remains unclear. Investigating the effects of wearing infrapatellar straps on quadriceps forces could enhance understanding of their role in managing OSD. Currently, studies related to OSD predominantly focus on males (Enomoto et al., 2021; Itoh et al., 2018; Takei et al., 2023; Watanabe et al., 2018). While some research suggests that OSD is more prevalent among boys (Enomoto et al., 2021; Enomoto et al., 2019), a previous study found no significant differences in OSD prevalence between female and male adolescents (de Lucena et al., 2011). Moreover, there has been an increasing trend in sports participation among adolescent females (Deng and Fan, 2022). Gender differences in lower extremity biomechanics have also been observed during running (Ferber et al., 2003). Therefore, research on the impact of wearing infrapatellar straps during physical activities, such as running, on the management of OSD in adolescent females is still lacking and necessary. Evaluating quadriceps forces when running with infrapatellar straps among adolescent females can offer a more comprehensive assessment of how the use of infrapatellar straps impacts the loads applied to the tibial tuberosity. Accordingly, the objective of this study was to quantitatively evaluate quadriceps forces when adolescent females perform running with and without infrapatellar straps. ParticipantsSixteen healthy adolescent females participated in this study, with an average age of 12.56 ± 0.96 years, body height of 1.62 ± 0.08 meters, and body weight of 51.47 ± 10.87 kg. The sample size for this study was determined by a priori analysis using G*Power 3.1.9.2 software (Heinrich-Heine-Universität Düsseldorf, Düsseldorf, Germany) (Faul et al., 2007). The alpha level and power (1 - β) were set to 0.05 and 0.8, respectively. The effect size (0.92) was set according to the result in the preliminary experiment. The preliminary experiment involved 8 participants (age: 12.50 ± 0.76 years, body height: 1.61 ± 0.07 m, body weight: 52.36 ± 13.20 kg). The mean and standard deviation values were 1.327 and 1.444, respectively. It was established that at least 12 participants were needed for the study. Therefore, sixteen adolescent females were recruited in the final analysis. All participants were right-leg dominant, meaning their right leg was the one most frequently used for kicking a ball. Each participant engaged in at least 90 minutes of physical activity per week. Participants with the following conditions will be excluded: (1) musculoskeletal injury within the past six months, (2) previous surgery on the lower extremities, (3) history of recurrent knee pain. The study was approved by the Science and Ethics Committee of the Beihang University (protocol code BM20200067), and written informed consent was obtained from all participants' guardians before the study began.
Experimental protocolParticipants were instructed to run under two conditions—wearing infrapatellar straps and not wearing them—in a randomized order. For the strapping session, the participants were fitted with commercial infrapatellar straps (AQAH236-1; Li-Ning Inc., Beijing, China) on both legs. According to the manufacturer's instructions and the location of OSD (Figure 1A), the infrapatellar strap was encircled around the leg just below the patella, with the rubber tubular member pressing on the patellar tendon (Figure 1B). All participants wore the same type of appropriately sized clothing and shoes. The clothing and shoes we provided were non-restrictive and fully exposed the electrode placement areas to support electromyography (EMG) measurements during movement.
Data recordingsKinematic data of participants running were collected using a ten-camera optical motion capture system (Vicon MX; Oxford Metrics, UK) at a sampling frequency of 100 Hz. A total of 32 infrared-reflective markers were placed on the torso, thighs, shanks, and feet to track the motion of each participant (Figure 1C). Ground reaction forces (GRFs) were recorded using two force plates (AMTI; Watertown, MA, USA) embedded into the walkway at a sampling rate of 1000 Hz. GRFs in the vertical, anteroposterior, and mediolateral directions were used for inverse dynamics simulations. Additionally, the vertical GRFs were applied to segment the gait cycle. Surface EMG data of vastus lateralis, vastus medialis, rectus femoris, biceps femoris long head, and soleus of right leg were recorded using a wireless EMG system (Trigno, Delsys; Boston, MA, USA) at 2000 Hz. All data were synchronized using Vicon Workstation v2.6 software. Before acquiring the EMG signals, the targeted skin areas were cleaned with alcohol to reduce contact impedance. Both the kinematic and GRF data were low-pass filtered at 15 Hz using a fourth-order zero-lag Butterworth filter (Maniar et al., 2020), using the software equipped with Vicon (Vicon Workstation v2.6). Prior to the recording session, participants completed a 10-minute warm-up run at their preferred speed to familiarize themselves with the experimental environment. Following this warm-up, each participant performed three practice trials along the walkway to determine their self-selected running speed. This speed, at which they felt comfortable running, was calculated by averaging the speeds recorded during these three trials. The speed was monitored via two sets of laser sensors placed before and after the force plates, spaced 4 meters apart. As participants passed the first and second sensors, the light beam was interrupted, triggering the start and end of the timing, respectively. The participant's running speed was then calculated based on the recorded time and the distance between the two sensors. the laser sensors were placed at shoulder height of each participant to avoid being triggered by arm swing. Participants were instructed to focus on an object on the front wall to avoid targeting the force plates while running (Abendroth-Smith, 1996; Queen et al., 2006). After each running trial, participants walked back to the starting position to prepare for the next trial. They were asked to rest if they reported feeling tired or appeared winded (Orendurff et al., 2018). The next trial would begin only when neither of these conditions persisted. A static trial was conducted for each participant, during which they stood in a neutral upright stance with their arms extended at a 45-degree angle from the body, feet shoulder-width apart, and eyes looking straight ahead. Then, three valid trials for each condition were recorded for each participant. The trial was considered valid if the running speed was within ± 5% of the self-selected speed, and the participants neither targeted nor missed the force plates. A 10-minute rest period was maintained after the completion of the three valid trials for one condition.
Musculoskeletal simulationThe inverse dynamics simulations in this study were conducted in OpenSim 4.4 (Delp et al., 2007) (Simbios, Stanford, CA, USA). A full-body musculoskeletal model, the Rajagopal model (2016), was used. The model included 80 muscle-tendon units and 17 torque actuators, and they were present in the lower body (40 per leg) and the upper body (one for each degree of freedom in the upper body), respectively (Rajagopal et al., 2016). Each muscle-tendon unit was represented with the improved Hill-type muscle model described by Millard et al. (2013). The unit included an active contractile element, a passive elastic element, a damper, and an elastic tendon (Millard et al., 2013). The force-generating capacity of each muscle-tendon unit was defined by normalized fiber force-length-velocity curves and tendon force-length curves (Millard et al., 2013). The viscoelasticity of the muscle was captured through the force-length curves and the damper element. A standard pipeline was employed to perform musculoskeletal simulations (Figure 1C). Static trial data was utilized to scale the Rajagopal model, which includes mass, segment size, and musculotendon lengths, to match each participant anthropometrically. The maximum isometric force of each lower-limb muscle was scaled by the ratio of the adolescent's body height (Hscaled) and body mass (Mscaled) to the generic model's body height (Hgeneric) and body mass (Mgeneric) according to the following equation (Hegarty et al., 2019):
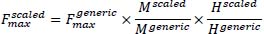 |
(1) |
where,  and and  are the maximum isometric force of each lower-limb muscle of scaled model and Rajagopal model, respectively. Then, marker trajectory data collected during running was used as input for the inverse kinematics algorithm, enabling the simulation to calculate joint angles, such as those of the hip, ankle, and knee, for each frame. Subsequently, dynamically consistent alignment between GRFs and model kinematics was achieved using a residual reduction algorithm. The computed muscle control algorithm was employed to calculate the muscle forces and muscle activity. are the maximum isometric force of each lower-limb muscle of scaled model and Rajagopal model, respectively. Then, marker trajectory data collected during running was used as input for the inverse kinematics algorithm, enabling the simulation to calculate joint angles, such as those of the hip, ankle, and knee, for each frame. Subsequently, dynamically consistent alignment between GRFs and model kinematics was achieved using a residual reduction algorithm. The computed muscle control algorithm was employed to calculate the muscle forces and muscle activity.
Parameter computationFor EMG, muscle forces, and muscle activity, three running cycles per condition for each participant were averaged. Parameters from the dominant leg were used. The dominant leg was used for analysis because biomechanical factors associated with a higher risk of OSD were observed in the dominant leg compared to the non-dominant leg (Wang et al., 1993). Raw EMG signals were band-pass filtered using a zero-lag, fourth-order Butterworth filter (20-450 Hz) (Gui and Zhang, 2016), rectified, and subsequently low-pass filtered (zero-lag, fourth-order Butterworth filter, 12 Hz) (Falisse et al., 2018) to obtain the EMG envelopes. The processed EMG data were then normalized by referring to peak values for each muscle activity in a gait cycle. Initial contact, toe-off, and the stance and swing phases of the gait cycle were determined based on the vertical component of the GRF and kinematic data (Novacheck, 1998). Specifically, Initial contact refers to the moment when the right foot contacts the force plate, while toe-off refers to the moment the right foot leaves the force plate. Both events were defined using a vertical GRF threshold of 10 N (Strike et al., 2018). The stance phase begins at initial contact and ends at toe-off, which marks the start of the swing phase of the gait cycle (Novacheck, 1998). The end of the swing phase is marked by the right foot contacting the force plate again. The timing of the second initial contact was determined using the marker trajectory of the right heel, drawing on the method described by Zhao et al. (2018), in combination with the vertical GRF component. The kinematic, GRF, and EMG data for each participant's gait cycle were interpolated to the same length before averaging. Quadriceps force was represented as the sum of the muscle forces of the rectus femoris, vastus lateralis, vastus medialis, and vastus intermedius. The continued tension of the quadriceps muscle was represented as the accumulated force of the quadriceps muscle. This force was defined as the area under the force-time curve throughout a cycle (∫ Fdt). Muscle forces were normalized to the participant's body weight (BW).
Validation of simulationIn this study, the muscle activity obtained from simulations under two conditions (with and without infrapatellar straps) was compared to the EMG data to validate the reliability of the inverse dynamics simulations. The study calculated the correlation between the peak EMG and peak muscle activity for the vastus lateralis, vastus medialis, rectus femoris, soleus, and biceps femoris long head during a gait cycle. Additionally, the correlation between the timing of the peak EMG and the timing of the peak muscle activity was also analyzed.
Statistical analysisThe analyzed variables, including peak forces of the quadriceps, rectus femoris, vastus lateralis, vastus medialis, vastus intermedius, soleus, and biceps femoris long head, and accumulated forces of the quadriceps, rectus femoris, vastus lateralis, vastus medialis, vastus intermedius, soleus, and biceps femoris long head were tested for normal distribution by using the Shapiro-Wilk test. For normally distributed variables, paired t-tests were performed to compare the peak and accumulated forces of the quadriceps, as well as the peak forces, accumulated forces, and peak active fiber forces of the vastus lateralis, vastus medialis, and vastus intermedius between the two conditions. The peak forces of rectus femoris and biceps femoris long head, as well as the accumulated forces of the rectus femoris, soleus and biceps femoris long head under conditions with and without infrapatellar straps were compared using the Wilcoxon signed-rank test, as the data were not normally distributed. The effect size was calculated using Cohen's d index and the following thresholds were used: 0.20 = small, 0.50 = moderate, 0.80 = large (Cohen, 1992). Data were statistically analyzed in SPSS 26 (IBM Corporation, NY, USA). Paired statistical parametric mapping (SPM) t-tests (Pataky, 2010) were used to analyze continuous parameters over time, specifically the muscle forces of the quadriceps, rectus femoris, vastus lateralis, vastus medialis, and vastus intermedius, as well as the active fiber forces of the vastus lateralis, vastus medialis, and vastus intermedius, throughout the gait cycle. The SPM analysis was conducted using an open-source SPM1D package (https://www.spm1d.org) in MATLAB (The MathWorks, Inc., Natick, Massachusetts, USA). The correlations between the timing of peak EMG activity and the timing of peak muscle activity during the full gait cycle were assessed using Spearman's correlation in SPSS 26. A correlation coefficient (r-value) significantly different from 0, with a p-value less than 0.05, indicates a considerable correlation (Yao et al., 2019). The reported statistical significance levels were all two-sided, and a p < 0.05 was deemed statistically significant.
As shown in Figure 2, the simulated muscle activity accurately reproduced the major features of the experimental EMG for the vastus lateralis, vastus medialis, rectus femoris, and soleus. However, some differences were observed between the simulated muscle activity and the EMG data in biceps femoris long head under both conditions, with and without straps (Figure 2A and Figure 2B). The peak simulated activity correlated with the peak EMG in the vastus lateralis, vastus medialis, rectus femoris, soleus, and biceps femoris long head under both conditions (r = -0.685, p = 0.029) (Figure 2C). The timing of peak activity was delayed compared to EMG but was significantly correlated in those muscles (r = 0.745, p = 0.013) (Figure 2D). The running speeds in the unstrapped and strapped conditions were 2.45 ± 0.18 m/s and 2.45 ± 0.21 m/s, respectively. No significant difference was observed in running speed between the two conditions (p = 0.916, d = 0.027). The peak quadriceps forces were significantly lower (p < 0.001, d = 1.338) with the use of infrapatellar straps (8.58 ± 1.40 BW) compared to without straps (9.96 ± 1.49 BW) (Figure 3A). For individual muscles within the quadriceps, the peak forces of the vastus muscles were significantly lower when running with infrapatellar straps compared to running without infrapatellar straps (p < 0.001, d = 1.427; p < 0.001, d = 1.951; and p < 0.001, d = 1.482 for vastus lateralis, vastus medialis, and vastus intermedius, respectively) (Figure 3C, Figure 3D and Figure 3E). The use of infrapatellar straps had no significant effect on the muscle forces of the rectus femoris, soleus, and biceps femoris long head (p = 0.321, d = 0.256; p = 0.289, d = 0.275; p = 0.088, d = 0.297, respectively) (Figure 3B, Figure 3F, and Figure 3G). For accumulated forces, paired t-test revealed significant differences in the accumulated forces of quadriceps (no-strap: 1312.78 ± 314.77 Ns, strap: 1178.02 ± 305.09 Ns), vastus lateralis (no-strap: 514.27 ± 113.08 Ns, strap: 444.78 ± 106.15 Ns), vastus medialis (no-strap:305.31 ± 72.58 Ns, strap: 274.45 ± 68.12 Ns), and vastus intermedius (no-strap:217.69 ± 55.57 Ns, strap: 199.89 ± 51.30 Ns) across all participants (p < 0.001, d = 1.201; p < 0.001, d = 1.322; p = 0.004, d = 0.862; and p = 0.015, d = 0.686, respectively) (Figure 4A, Figure 4C, Figure 4D, and Figure 4E). Wearing infrapatellar straps significantly reduced accumulated forces of the biceps femoris long head (p = 0.007, d = 0.513) (Figure 4G). It had no significant effect on accumulated forces of the rectus femoris and soleus (p = 0.501, d = 0.162; p = 1.000, d = 0.120, respectively) (Figure 4B and Figure 4F). The SPM results showed that quadriceps forces were significantly lower during the stance phase of the gait cycle (between 11.99% and 17.44%) under strapped condition compared to the unstrapped condition, where it exceeded the critical t-statistic threshold at p = 0.003 (Figure 5A and Figure 5B). In the individual muscles within the quadriceps, the muscle forces of vastus lateralis, vastus medialis, and vastus intermedius were significantly reduced in the stance phase when using infrapatellar straps (between 13.39% and 20.47%, 12.8% and 17.83%, and 12.75% and 15.81% of the running cycle, p < 0.002, p = 0.003, and p = 0.016, respectively) (Figure 5D, Figure 5E and Figure 5F). There was no significant difference in the rectus femoris muscle forces throughout the entire gait cycle between the strapped and unstrapped conditions (Figure 5C). The peak active fiber forces in the vastus lateralis, vastus medialis, and vastus intermedius were significantly reduced during running with infrapatellar straps (p < 0.001, d = 1.382; p < 0.001, d = 1.839; p < 0.001, d = 1.346, respectively) (Figure 6A, Figure 6B and Figure 6C). When wearing infrapatellar straps, the active fiber forces of the vastus lateralis, vastus medialis, and vastus intermedius decreased by 13.60% - 20.75%, 12.92% - 17.94%, and 12.77% - 15.91% of the running cycle, respectively (p < 0.001, p = 0.002, and p = 0.015) (Figure 6D, Figure 6E and Figure 6F). However, infrapatellar straps had minimal impact on the passive fiber forces, normalized fiber length, and normalized fiber velocity of these muscles. This study investigated the effect of wearing infrapatellar straps on quadriceps forces in adolescent females during running, aiming to evaluate the effectiveness of infrapatellar straps in the prevention and treatment of OSD. The results showed that the use of infrapatellar straps was associated with reduced peak and accumulated forces of the quadriceps. Wearing infrapatellar straps during running has a greater impact on the vastus muscles than on the rectus femoris, with the reduction in muscle forces primarily occurring during the stance phase. The results indicate that wearing infrapatellar straps may help lower the forces on tibial tuberosity by decreasing vastus muscle forces during the stance phase, which could be beneficial for managing OSD. Adolescents who need to reduce excessive rectus femoris forces caused by a shortened or tight rectus femoris, which may be associated with the occurrence of OSD, may experience limited benefits from wearing infrapatellar straps. In our study, the reliability of inverse dynamics simulation was validated by comparison with EMG data. EMG, as a noninvasive method, provides both direct and indirect information about muscle electrical activity (Karimi et al., 2021) and is widely used for assessing muscle activation (Disselhorst-Klug et al., 2009; Heintz and Gutierrez-Farewik, 2007). In the current study, under both strapped and unstrapped conditions, the peak simulated muscle activations exhibited a strong correlation with the peak EMG values. Additionally, the timing of peak simulated activation and peak EMG also demonstrated a strong correlation, further validating the reliability of the simulation. A delay between simulated muscle activity and EMG found in this study was consistent with Corcos et al.'s (1992) findings, which consist of transport time and the time needed to generate detectable force changes (Corcos et al., 1992). The differences between simulated muscle activations and EMG data in the biceps femoris long head may result from soft tissue interference during EMG measurements. Achieving simulated activations that accurately reflect measured EMG across all muscles remains a challenge in muscle-driven simulation studies (Rajagopal et al., 2016). This study examined a key factor in the occurrence of OSD: the maximum force of the quadriceps, which decreases when wearing infrapatellar straps during running. OSD is an avulsion of a small portion of the tibial tuberosity caused by a violent contraction of the quadriceps extensor mechanism (Uzunov, 2008). Katoh (1988) reported a positive relationship between the force generated by the quadriceps muscle as an etiologic factor of OSD. Thus, this study evaluated peak quadriceps forces while wearing infrapatellar straps during running to clarify the effectiveness of the straps in managing OSD. The reduced peak quadriceps forces when wearing infrapatellar straps suggest that infrapatellar straps can help lower the maximum traction force on the tibial tuberosity, thereby potentially decreasing the risk of OSD onset in adolescent females and contributing to its prevention. This study also examined another important factor in the occurrence of OSD: the continuous traction of the quadriceps, characterized by the accumulated forces of quadriceps forces, which was shown to be reduced by wearing infrapatellar straps. In addition to the violent traction of the quadriceps, the continuous traction applied on the tibial tuberosity is also considered to be related to the onset and aggravation of OSD (Gholve et al., 2007; Pan et al., 2022). This suggests that accumulated forces throughout the gait cycle should be considered when evaluating the effectiveness of infrapatellar straps in managing OSD. The reduction in accumulated forces when wearing infrapatellar straps during running suggests that infrapatellar straps may help decrease the continuous traction applied to the tibial tuberosity, thereby potentially benefiting the prevention of OSD in adolescent females. The reduction in accumulated forces was associated with decreased quadriceps forces during the stance phase of the gait cycle while wearing infrapatellar straps during running, suggesting that infrapatellar straps may specifically reduce the load during critical phases of the gait cycle. Baltaci et al. (2004) reported that the injury mechanism of the tibial tuberosity apophysis is due to the eccentric contraction force of the quadriceps exceeding its strength. The reduction in quadriceps forces during the stance phase while wearing infrapatellar straps may help decrease traction on the tibial tuberosity, thereby lowering the risk of damage and benefiting the prevention of OSD. Wearing infrapatellar straps has a considerable impact on the vastus muscle forces within the quadriceps, resulting in a significant reduction in muscle forces, accumulated forces, and muscle forces in the stance phase. The vastus lateralis is the largest quadriceps muscle with high force-generating potential (Bohm et al., 2021), and in this study, its muscle forces exceed those of the other quadriceps heads. The vastus medialis and the vastus intermedius operate similarly to the vastus lateralis since they share the same single patellar tendon (Bohm et al., 2021). Therefore, the use of infrapatellar straps has a similar impact on the vastus muscles. The reduction in vastus muscle forces was primarily attributed to a decrease in active fiber forces. Since infrapatellar straps had minimal effects on passive fiber forces, normalized fiber length, and velocity, the observed reduction was likely due to decreased muscle activation caused by the strap. Earl et al. (2004) reported that the vastus lateralis and vastus medialis were significantly less active when using a brace. Rosen et al. (2017) found that the use of infrapatellar straps significantly reduces the muscle activity of the vastus lateralis. Muscle force production is initiated by electrophysiological activation (Disselhorst-Klug et al., 2009), suggesting that the reductions in vastus muscle forces when wearing infrapatellar straps may result from decreased muscle activity. The lower muscle activity when using infrapatellar straps may be explained by (i) fewer fibers being activated during the stance phase, (ii) external pressure changing the length of the vastus muscles and allowing for more efficient contraction, and (iii) other motor units within the vastus muscles or other muscles offering a greater contribution to running (Earl et al., 2004; Snyder-Mackler and Epler, 1989). It is noteworthy that wearing infrapatellar straps has little impact on the rectus femoris muscle forces. In Earl's study, wearing straps does not significantly affect the muscle activity of the rectus femoris (Earl et al., 2004). OSD typically develops in adolescents aged 8-14 in females and 10-15 in males (Itoh et al., 2018), coinciding with the developmental phase of the tibial tuberosity and related growth spurts. During this rapid growth stage, the relatively rapid lengthening of the femur in relation to the quadriceps muscle, particularly the rectus femoris muscle, increases the risk of OSD (Neuhaus et al., 2021). Well-developed and inelastic rectus femoris muscle imparts additional tensile forces on the tibial tuberosity and may influence the onset and development of OSD. The results of this study suggest that the effectiveness of using infrapatellar straps when running may be limited for OSD patients with a rectus femoris-induced pathology and in adolescents with inflexible rectus femoris. Moreover, 5 out of 24 knees (21%) examined did not experience relief from symptoms of OSD after using infrapatellar straps in Levine's study (1981). These five male adolescents, aged between 11 and 15, were at an age when growth spurts are common, leading us to speculate that rectus femoris-induced pathology might be responsible for the lack of symptomatic relief. The findings reveal that the development of the rectus femoris muscle, such as its flexibility, should be examined before choosing infrapatellar straps for the conservative treatment or prevention of OSD. The impact of infrapatellar straps on the continuous and maximum tractions of the biceps femoris long head, an agonist and antagonistic muscle of the quadriceps, was also investigated. The biceps femoris long head is one of the muscle heads that comprise the hamstrings (Nakao et al., 2018). As agonist and antagonist muscles, close collaboration between the quadriceps and hamstring muscles is integral to maintaining knee joint stability during movement (Wu et al., 2017). According to the findings in our study, quadriceps forces reached their peak at around 15% of the gait cycle, while the biceps femoris long head were not at their most active during this phase. Therefore, the limited effect of infrapatellar straps on the peak muscle forces of the biceps femoris long head observed in this study could be explained. Strength imbalances between agonist and antagonist muscles may increase the risk of injury to the lower extremity (Lutz et al., 2023). Hence, infrapatellar straps can reduce the accumulated forces of quadriceps without major alterations in the agonist-antagonist muscle balance, which is essential for their effective application. Additionally, the reduction in accumulated forces on both the quadriceps and biceps femoris long head may influence the energetics of lower extremity joints during running, potentially helping to reduce energy costs. Limited effects of infrapatellar straps on the soleus were observed in this study. As one of the primary ankle plantar flexors, the soleus plays a vital role in locomotion and contributes significantly to the force necessary for vertical support and forward progression during running (Lai et al., 2015). The minimal impact of infrapatellar straps on the forces of the soleus suggests that the use of infrapatellar straps has little effect on plantarflexion of the foot during the middle and terminal stance phases. In the current study, only adolescent females were recruited, as previous research on OSD has primarily focused on males (Enomoto et al., 2021; Itoh et al., 2018; Takei et al., 2023; Watanabe et al., 2018) and similar incidence rates of OSD for both genders (de Lucena et al., 2011). To our knowledge, the only study examining the efficacy of infrapatellar straps for OSD. Levine and Kashyap (1981) investigated the effectiveness of infrapatellar straps on 17 adolescent males and 2 adolescent females with OSD, finding that while the straps benefited the females, their efficacy was limited for five males. The average age of these five males was 12.8 years, coinciding with their second peak growth spurt around age 13 (Ohtaka et al., 2020). This growth phase may contribute to the onset of OSD (Takei et al., 2023), as the asynchronous development of bone and quadriceps muscle, particularly the rectus femoris, during this phase (Neuhaus et al., 2021; Ross and Villard, 2003), thereby explaining the limited effects observed in those five males. Additionally, Dar and Mei-Dan (2019) examined the management of infrapatellar straps on knee pain in male adolescent athletes, revealing that infrapatellar straps reduced local pain during jumps. Furthermore, Rosen et al. (2017) investigated the impact of infrapatellar straps on quadriceps muscle activity in male adults. Their findings indicated that the straps reduced activity in the vastus lateralis, while the effect on rectus femoris muscle activity was limited. Given that higher EMG levels correspond to greater muscle force development (Disselhorst-Klug et al., 2009), infrapatellar straps may help reduce tensile stress on the tendon (Rosen et al., 2017). While our results are generally consistent with previous research, future studies should analyze the effects of wearing infrapatellar straps on quadriceps forces during running in adolescent males due to the gender differences in lower extremity biomechanics during running (Ferber et al., 2003). This study had a few limitations. Firstly, only healthy adolescents were enrolled in this study. According to the literature, running poses a high risk for the onset of OSD (Takei et al., 2023). Recruiting OSD patients for the study could exacerbate their symptoms. This study aimed to investigate the changes in quadriceps forces between two strapping conditions instead of the absolute values of the loads. The results provided baseline data that will be beneficial for future studies in the symptomatic population. Nevertheless, symptomatic patients should be considered in future studies. Secondly, the study was conducted on adolescent females, which may limit its generalizability to adolescent males. Future studies are needed to examine the immediate effects of infrapatellar straps on quadriceps forces in adolescent males. Thirdly, the flexibility of the participants' rectus femoris or quadriceps muscles was not measured, despite our findings suggesting that muscle flexibility may influence the effectiveness of infrapatellar straps. The flexibility of the participants' rectus femoris and quadriceps should be measured in the future to provide more comprehensive understanding of the effects of infrapatellar straps. Finally, only self-selected running was included in this study. Future studies should explore the impact of wearing infrapatellar straps during different types of motions that associated with the onset of OSD, such as jumping and kicking, to verify and supplement our findings. In conclusion, wearing infrapatellar straps during running could reduce the peak and accumulated forces of the quadriceps, decreasing the high and continued traction applied to the tibial tuberosity. This significant reduction in forces is strongly associated with decreased vastus muscle forces during the stance phase, suggesting that infrapatellar straps may be particularly beneficial for adolescents needing to reduce excessive vastus muscle forces, thus contributing to the treatment and prevention of OSD. Due to the minimal impact of wearing infrapatellar straps on rectus femoris muscle forces, their effectiveness may be limited for adolescents needing to reduce excessive rectus femoris forces caused by a shortened or tight muscle. This study can help clarify the indications and principles of rehabilitation with infrapatellar straps, providing new insights into their protective effects against OSD.
| ACKNOWLEDGEMENTS |
This work was supported by the National Natural Science Foundation of China [grant number 12072019]. The experiments comply with the current laws of the country in which they were performed. The authors have no conflict of interest to declare. The datasets generated and analyzed during the current study are not publicly available but are available from the corresponding author upon reasonable request, who was an organizer of the study. |
|
| AUTHOR BIOGRAPHY |
|
 |
Xueying Zhang |
| Employment: School of Biological Science and Medical Engineering, Beihang University, Beijing, China |
| Degree: MSc |
| Research interests: Knee biomechanics, Rehabilitation engineering, Sport sciences |
| E-mail: zxy15810113196@163.com |
| |
 |
Weiyan Ren |
| Employment: Associate Professor, School of Engineering Medicine, Beihang University, Beijing, China |
| Degree: PhD |
| Research interests: Biomechanics, Rehabilitation engineering |
| E-mail: renweiyan@buaa.edu.cn |
| |
 |
Xingyue Wang |
| Employment: School of Biological Science and Medical Engineering, Beihang University, Beijing, China |
| Degree: BSc |
| Research interests: Knee biomechanics, Rehabilitation engineering, Sport biomechanics |
| E-mail: wangxingyue@buaa.edu.cn |
| |
 |
Jie Yao |
| Employment: Associate Professor, School of Biological Science and Medical Engineering, Beihang University, Beijing, China |
| Degree: PhD |
| Research interests: Biomechanics, Rehabilitation engineering, Sport sciences |
| E-mail: astromilk@163.com |
| |
 |
Fang Pu |
| Employment: Professor, School of Biological Science and Medical Engineering, Beihang University, Beijing, China |
| Degree: PhD |
| Research interests: Biomechanics, Rehabilitation engineering, Sport sciences |
| E-mail: pufangbme@buaa.edu.cn |
| |
|
| |
| REFERENCES |
 Abendroth-Smith J (1996) Stride adjustments during a running approach toward a force plate. Research Quarterly for Exercise and Sport 67, 97-101. Crossref |
 Adirim T.A., Cheng T.L. (2003) Overview of injuries in the young athlete. Sports Medicine 33, 75-81. Crossref |
 Baltaci G., Özer H., Tunay V.B. (2004) Rehabilitation of avulsion fracture of the tibial tuberosity following Osgood-Schlatter disease. Knee Surgery, Sports Traumatology, Arthroscopy 12, 115-118. Crossref |
 Bezuglov E., Tikhonova А., Chubarovskiy P.V., Repetyuk А., Khaitin V., Lazarev A., Usmanova E. (2020) Conservative treatment of Osgood-Schlatter disease among young professional soccer players. International Orthopaedics 44, 1737-1743. Crossref |
 Bohm S., Mersmann F., Santuz A., Schroll A., Arampatzis A. (2021) Muscle-specific economy of force generation and efficiency of work production during human running. Elife 10, e67182. Crossref |
 Cohen J (1992) Statistical power analysis. Current Directions in Psychological Science 1, 98-101. Crossref |
 Corcos D.M., Gottlieb G.L., Latash M.L., Almeida G.L., Agarwal G.C. (1992) Electromechanical delay: An experimental artifact. Journal of Electromyography and Kinesiology 2, 59-68. Crossref |
 Dar G., Mei-Dan E. (2019) Immediate effect of infrapatellar strap on pain and jump height in patellar tendinopathy among young athletes. Prosthetics and Orthotics International 43, 21-27. Crossref |
 de Lucena G.L., dos Santos Gomes C., Guerra R.O. (2011) Prevalence and associated factors of Osgood-Schlatter syndrome in a population-based sample of brazilian adolescents. American Journal of Sports Medicine 39, 415-420. Crossref |
 Delp S.L., Anderson F.C., Arnold A.S., Loan P., Habib A., John C.T., Guendelman E., Thelen D.G. (2007) OpenSim: open-source software to create and analyze dynamic simulations of movement. IEEE Transactions on Biomedical Engineering 54, 1940-1950. Crossref |
 Deng Y., Fan A. (2022) Trends in sports participation in adolescents: Data from a large-scale sample in the us adolescents. Frontiers in Public Health 10, 960098. Crossref |
 Disselhorst-Klug C., Schmitz-Rode T., Rau G. (2009) Surface electromyography and muscle force: Limits in Semg-force relationship and new approaches for applications. Clinical Biomechanics 24, 225-235. Crossref |
 Earl J.E., Piazza S.J., Hertel J. (2004) The protonics knee brace unloads the quadriceps muscles in healthy subjects. Journal of Athletic Training 39, 44-49. |
 Enomoto S., Oda T., Sugisaki N., Toeda M., Kurokawa S., Kaga M. (2021) Muscle stiffness of the rectus femoris and vastus lateralis in children with Osgood-Schlatter disease. The Knee 32, 140-147. Crossref |
 Enomoto S., Tsushima A., Oda T., Kaga M. (2019) The characteristics of the muscle-tendon unit in children affected by Osgood-Schlatter disease. Translational Sports Medicine 2, 196-202. Crossref |
 Falisse A., Van Rossom S., Gijsbers J., Steenbrink F., van Basten B.J.H., Jonkers I., van den Bogert A.J., De Groote F. (2018) OpenSim versus human body model: A comparison study for the lower limbs during gait. Journal of Applied Biomechanics 34, 496-502. Crossref |
 Faul F., Erdfelder E., Lang A.-G., Buchner A. (2007) G*power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods 39, 175-191. Crossref |
 Ferber R., Davis I.M., Williams D.S. (2003) Gender differences in lower extremity mechanics during running. Clinical Biomechanics 18, 350-357. Crossref |
 Gholve P.A., Scher D.M., Khakharia S., Widmann R.F., Green D.W. (2007) Osgood Schlatter syndrome. Current Opinion in Pediatrics 19, 44-50. Crossref |
 Gui K., Zhang D. (2016) Influence of locomotion speed on biomechanical subtask and muscle synergy. Journal of Electromyography and Kinesiology 30, 209-215. Crossref |
 Guldhammer C., Rathleff M.S., Jensen H.P., Holden S. (2019) Long-term prognosis and impact of Osgood-Schlatter disease 4 years after diagnosis: A retrospective study. Orthopaedic Journal of Sports Medicine, 7. Crossref |
 Hegarty A.K., Hulbert T.V., Kurz M.J., Stuberg W., Silverman A.K. (2019) Evaluation of a method to scale muscle strength for gait simulations of children with cerebral palsy. Journal of Biomechanics 83, 165-173. Crossref |
 Heintz S., Gutierrez-Farewik E.M. (2007) Static optimization of muscle forces during gait in comparison to EMG-to-force processing approach. Gait & Posture 26, 279-288. Crossref |
 Itoh G., Ishii H., Kato H., Nagano Y., Hayashi H., Funasaki H. (2018) Risk assessment of the onset of Osgood-Schlatter disease using kinetic analysis of various motions in sports. Plos One 13, e0190503. Crossref |
 Karimi M.T., Hemmati F., Mardani M.A., Sharifmoradi K., Hosseini S.I., Fadayevatan R., Esrafilian A. (2021) Determination of the correlation between muscle forces obtained from OpenSim and muscle activities obtained from electromyography in the elderly. Physical and Engineering Sciences in Medicine 44, 243-251. Crossref |
 Katoh K (1988) An analysis of quadriceps muscle force in boys with Osgood-Schlatter disease. Nihon Seikeigeka Gakkai Zasshi 62, 523-533. |
 Ladenhauf H.N., Seitlinger G., Green D.W. (2020) Osgood-Schlatter disease: A 2020 update of a common knee condition in children. Current Opinion in Pediatrics 32, 107-112. Crossref |
 Lai A., Lichtwark G.A., Schache A.G., Lin Y.C., Brown N.A.T., Pandy M.G. (2015) In vivo behavior of the human soleus muscle with increasing walking and running speeds. Journal of Applied Physiology 118, 1266-1275. Crossref |
 Lavagnino M., Arnoczky S.P., Dodds J., Elvin N. (2011) Infrapatellar straps decrease patellar tendon strain at the site of the jumper's knee lesion: A computational analysis based on radiographic measurements. Sports Health 3, 296-302. Crossref |
 Levine J., Kashyap S. (1981) A new conservative treatment of Osgood-Schlatter disease. Clinical Orthopaedics and Related Research 158, 126-128. Crossref |
 Lutz F.D., Cleary C.J., Moffatt H.M., Sullivan V.E., LaRoche D.P., Cook S.B. (2023) Comparison of the h:Q ratio between the dominant and nondominant legs of soccer players: A meta-analysis. Sports Health 15, 486-496. Crossref |
 Maniar N., Schache A.G., Pizzolato C., Opar D.A. (2020) Muscle contributions to tibiofemoral shear forces and valgus and rotational joint moments during single leg drop landing. Scandinavian Journal of Medicine & Science in Sports 30, 1664-1674. Crossref |
 Millard M., Uchida T., Seth A., Delp S.L. (2013) Flexing computational muscle: Modeling and simulation of musculotendon dynamics. Journal of Biomechanical Engineering 135, 021005. Crossref |
 Mital M.A., Matza R.A. (1977) Osgood-Schlatter disease: The painful puzzler. The Physician and Sportsmedicine 5, 60-73. Crossref |
 Nakao G., Taniguchi K., Katayose M. (2018) Acute effect of active and passive static stretching on elastic modulus of the hamstrings. Sports Medicine International Open 2, 163-170. Crossref |
 Neuhaus C., Appenzeller-Herzog C., Faude O. (2021) A systematic review on conservative treatment options for Osgood-Schlatter disease. Physical Therapy in Sport 49, 178-187. Crossref |
 Novacheck T.F. (1998) The biomechanics of running. Gait & Posture 7, 77-95. Crossref |
 Ohtaka M., Hiramoto I., Minagawa H., Matsuzaki M., Saito A., Ishigoka M. (2020) Musculoskeletal examination of junior high school students using a diagnostic ultrasound device: Investigation of Osgood-Schlatter disease and its related factors. Journal of Physical Fitness and Sports Medicine 9, 105-113. Crossref |
 Orendurff M.S., Kobayashi T., Tulchin-Francis K., Tullock A.M.H., Villarosa C., Chan C., Strike S. (2018) A little bit faster: Lower extremity joint kinematics and kinetics as recreational runners achieve faster speeds. Journal of Biomechanics 71, 167-175. Crossref |
 Pan T., Mun F., Martinazzi B., King T.S., Petfield J.L., Hennrikus W.L. (2022) The posterior tibial slope and insall-salvati index in operative and nonoperative adolescent athletes with Osgood-Schlatter disease. Archives of Orthopaedic and Trauma Surgery 142, 3903-3907. Crossref |
 Pataky T.C. (2010) Generalized n-dimensional biomechanical field analysis using statistical parametric mapping. Journal of Biomechanics 43, 1976-1982. Crossref |
 Queen R.M., Gross M.T., Liu H.Y. (2006) Repeatability of lower extremity kinetics and kinematics for standardized and self-selected running speeds. Gait & Posture 23, 282-287. Crossref |
 Rajagopal A., Dembia C.L., DeMers M.S., Delp D.D., Hicks J.L., Delp S.L. (2016) Full-body musculoskeletal model for muscle-driven simulation of human gait. IEEE Transactions on Biomedical Engineering 63, 2068-2079. Crossref |
 Rathleff M.S., Winiarski L., Krommes K., Graven-Nielsen T., Hölmich P., Olesen J.L., Holden S., Thorborg K. (2020) Activity modification and knee strengthening for Osgood-Schlatter disease: A prospective cohort study. Orthopaedic Journal of Sports Medicine, 8. Crossref |
 Rosen A.B., Ko J., Simpson K.J., Brown C.N. (2017) Patellar tendon straps decrease pre-landing quadriceps activation in males with patellar tendinopathy. Physical Therapy in Sport 24, 13-19. Crossref |
 Ross M.D., Villard D. (2003) Disability levels of college-aged men with a history of Osgood-Schlatter disease. Journal of Strength and Conditioning Research 17, 659-663. Crossref |
 Snyder-Mackler L., Epler M. (1989) Effect of standard and aircast tennis elbow bands on integrated electromyography of forearm extensor musculature proximal to the bands. American Journal of Sports Medicine 17, 278-281. Crossref |
 Strike S.C., Arcone D., Orendurff M. (2018) Running at submaximal speeds, the role of the intact and prosthetic limbs for trans-tibial amputees. Gait & Posture 62, 327-332. Crossref |
 Takei S., Torii S., Taketomi S., Iizuka S., Tojima M., Iwanuma S., Iida Y., Tanaka S. (2023) Developmental stage and lower quadriceps flexibilities and decreased gastrocnemius flexibilities are predictive risk factors for developing Osgood-Schlatter disease in adolescent male soccer players. Knee Surgery, Sports Traumatology, Arthroscopy 31, 3330-3338. Crossref |
 Toonstra J., Cripps A. (2020) The effectiveness of an infrapatellar strap on reducing pain associated with patellar tendinopathy. Journal of Sports Medicine Allied Health Sciences: Official Journal of the Ohio Athletic Trainers Association 5, 1. Crossref |
 Uzunov V (2008) A look at the pathophysiology and rehabilitation of Osgood-Schlatter syndrome. Gym Coach 2, 39-45. |
 Wang S.S., Whitney S.L., Burdett R.G., Janosky J.E. (1993) Lower extremity muscular flexibility in long distance runners. Journal of Orthopaedic and Sports Physical Therapy 17, 102-107. Crossref |
 Watanabe H., Fujii M., Yoshimoto M., Abe H., Toda N., Higashiyama R., Takahira N. (2018) Pathogenic factors associated with Osgood-Schlatter disease in adolescent male soccer players: A prospective cohort study. Orthopaedic Journal of Sports Medicine, 6. Crossref |
 Wu R., Delahunt E., Ditroilo M., Lowery M.M., De Vito G. (2017) Effect of knee joint angle and contraction intensity on hamstrings coactivation. Medicine & Science in Sports & Exercise 49, 1668-1676. Crossref |
 Yao J., Guo N., Xiao Y., Li Z., Li Y., Pu F., Fan Y. (2019) Lower limb joint motion and muscle force in treadmill and over-ground exercise. Biomedical Engineering Online 18, 89. Crossref |
 Zhao W., Song W., Rao J.S., Wei R.H., Li L.F., Ji R., Zhao C., Yang Z.Y., Li X.G. (2018) Gait division of healthy and spinal cord-injured rhesus monkeys by one-dimensional toe signals. Journal of Mechanics in Medicine and Biology , 18. Crossref |
|
| |
|
|
|
|

